Author: JoAnn Pushkin
Breast Cancer Awareness Month is here and a good time to educate women on an important aspect in the detection of breast cancer: breast density. The purpose of breast cancer screening is to detect cancer earlier than it would otherwise be found. When breast cancer is found early, it means less aggressive treatment will be needed and survival rates are highest. Multiple studies have proven that early detection of cancers by mammography reduces breast cancer deaths in women aged 40 to 74.
However, mammography is more effective in detecting cancers in some women than others. For women
with dense breasts, cancer often goes unseen on mammography and therefore, additional screening may be needed.
Dense Breast Fast Facts:
- Breast density is determined through a woman’s mammogram and described as one of four categories depending on the amount of breast tissue in comparison to fat in the breast.
- 40% of women age 40 and over have dense breasts.
- Cancer is 4-6 times more likely in women with extremely dense breasts than in women with the least dense breasts.
- Though mammograms find some cancers not seen on other screening tests, in dense breasts, mammograms will miss more than 50% of the cancers present.
- Other screening tests, such as ultrasound or breast MRI, in addition to mammography substantially increase detection of early stage breast cancer in dense breasts.
Why does breast density matter?
Dense breasts both increase the likelihood of developing breast cancer and of that cancer being missed by mammography.
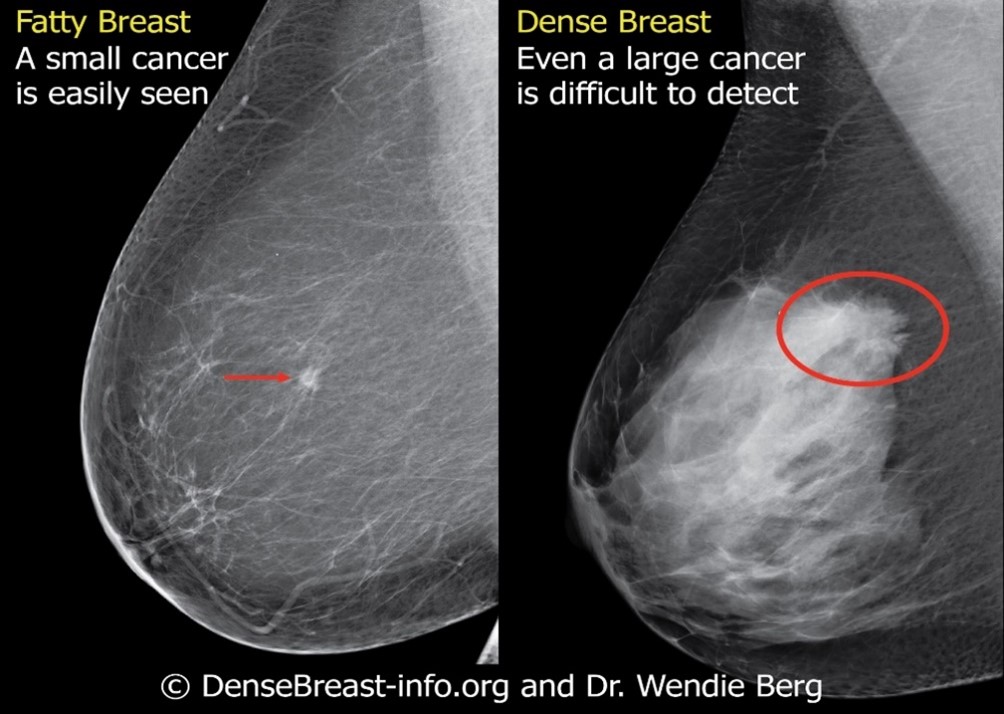
In order to understand how cancers may be masked by dense tissue on a mammogram, it is important to understand the way cancer is seen on a mammogram. Dense breast tissue shows up as white on a mammogram, while fatty tissue is dark. Unfortunately, cancers also tend to be white spots on a mammogram. If there is a lot of dense tissue on a mammogram, a cancer can be “hiding” among the dense tissue. This is true even if the mammogram was done with 3D/tomosynthesis. Looking for a cancer in a dense breast has been compared to looking for a snowball in a blizzard.
It is important to understand that a “normal,” “negative,” or “benign” mammogram does not necessarily mean cancer is not present. No matter how recent your last mammogram, a lump or any changes in your breast should be brought to the attention of your health provider.

In addition to hiding cancer, breast density is also one of many known risk factors for breast cancer. The greater the density of the breast tissue, the higher the risk for developing breast cancer. Women with
extremely dense breast tissue have a 4-6 times increased risk of developing breast cancer compared to women with fatty breasts. However, the majority of women fall in between these extremes.
What is breast density?
There is a wide range of normal appearances to women’s breasts, both visually and on mammography. All breasts are made up of a mix of glandular and fibrous tissue (referred to as “dense” tissue), and fat. Breast density is determined by the relative amounts of fatty and dense tissue on a mammogram, and is unique to each woman. Women who have a higher proportion of dense tissue compared to fatty tissue are considered to have “dense” breasts. Your breast density is determined by the radiologist who examines your mammography images, and is not based on how a breast looks or feels.
Is breast density common?
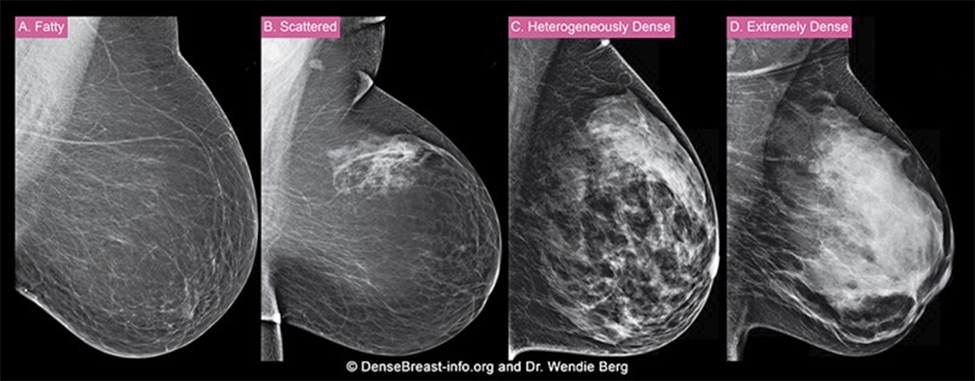
Yes, dense breast tissue is very common, in fact, 40% of women of age 40 and over have dense breasts. When you have your mammogram, your breast density is rated into one of four categories:
- Category A – Fatty
- Category B – Scattered areas of fibroglandular density
- Category C – Heterogeneously dense
- Category D – Extremely dense

Breasts which are Category C – Heterogeneously dense, or Category D – Extremely dense, are considered to be “dense” breasts.
How do I know if I have dense breasts?
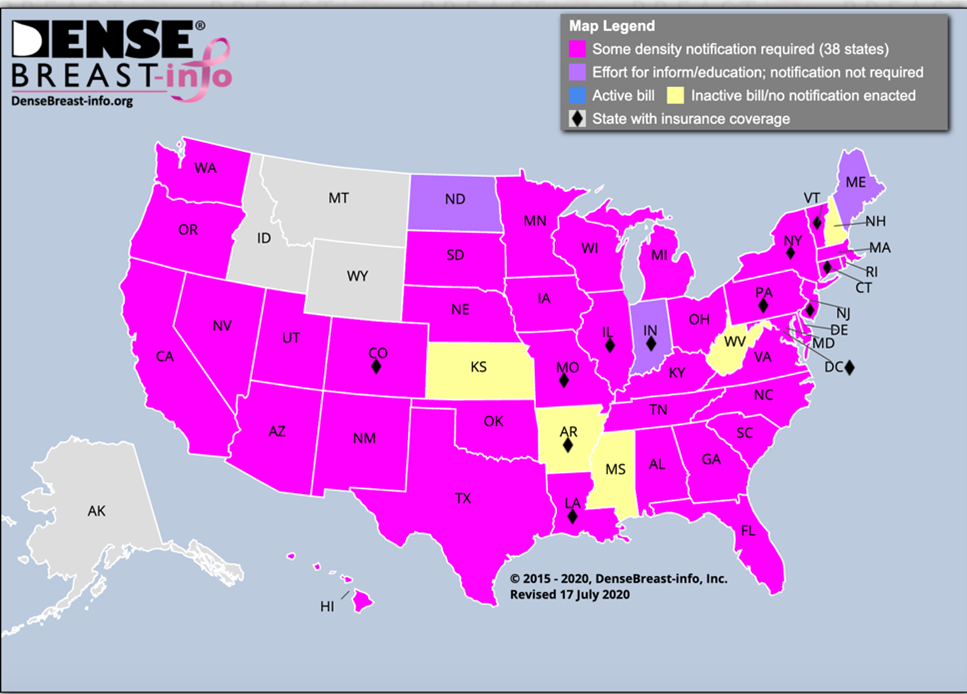
Breast density is included in the mammogram report to your referring provider. Generally, this information will be provided to you by your health care provider and it may also be included in the results letter you receive after your mammogram is performed. Many states, thirty-eight in total, as well as the District of Columbia, now have laws that require some level of information about breast density be included in the letter women receive after their mammogram. However, the laws vary from state-to-state, so it is important to be aware of the specific law in your state. Federal legislation has been passed, which directs the Food and Drug Administration (FDA) to develop standardized reporting language that all states will adhere to, but no federal requirement is in effect just yet.
To understand what the reporting requirements are in your state, please see the interactive legislative map on DenseBreast-info.org.
Can I change my breast density through diet? Exercise?
Weight loss?
Diet, exercise, and weight loss are not directly related to breast density, and do not have any effect on the amount of dense tissue in your breast. However, as with other parts of your body, if you gain weight,
there will be more fat, and if you lose weight, there will be less. Since breast density is determined by the comparison of fatty tissue to dense tissue, weight loss or gain can affect how fatty or how dense your breasts look on a mammogram (even if the amount of dense tissue has not changed).

What are other screening options?
Mammography is the standard screening test for all women, and is proven to reduce deaths due to breast cancer. In women with dense breasts, it may be beneficial to consider supplemental screening in addition to
mammography. Depending on your age, your risk level (determined by a health provider), and your breast density, additional screening tests, such as ultrasound for women at average risk, or MRI for women at high risk or with a personal history or breast cancer, may be recommended. Though most women being screened will not have breast cancer, these supplemental screening tools have been shown to improve the detection of early-stage breast cancer in women with dense breasts. With any screening, there is also the
possibility of being called back for additional testing for a finding that is not cancer. Insurance coverage varies for supplemental screening.
Early detection matters, so be an informed self-advocate. All women should know their breast density status and individual risk factors, know whether they are determined to be “high risk,” and discuss the benefits and risks of supplemental screening with their health care professional to ensure the earliest stage diagnosis possible.
©DenseBreast-info.org
Additional resources:
Patient Video Series: Let’s Talk About Dense Breasts
About the author:
JoAnn Pushkin, Executive Director, DenseBreast-info.org, learned of her own breast density’s masking effect on her mammogram after finding a palpable lump which went undetected by mammography several years in a row. Ms. Pushkin’s initiative and advocacy served as inspiration for New York State’s Breast
Density Inform law. On the federal level, Ms. Pushkin led the efforts for both the introduction of the Federal Breast Density and Mammography Reporting Act, as well as the FDA’s Mammography Quality Standards Act regulatory amendment consideration.
